Luteal Phase Defect (LPD) is a hormonal condition that affects the second half of a woman’s menstrual cycle, known as the luteal phase. This phase occurs after ovulation and is crucial for preparing the uterine lining for implantation and supporting early pregnancy. In women with LPD, the corpus luteum, which forms from the ruptured follicle after ovulation, does not produce enough progesterone. As a result, the uterine lining may not develop adequately, making implantation difficult and increasing the risk of early miscarriage.
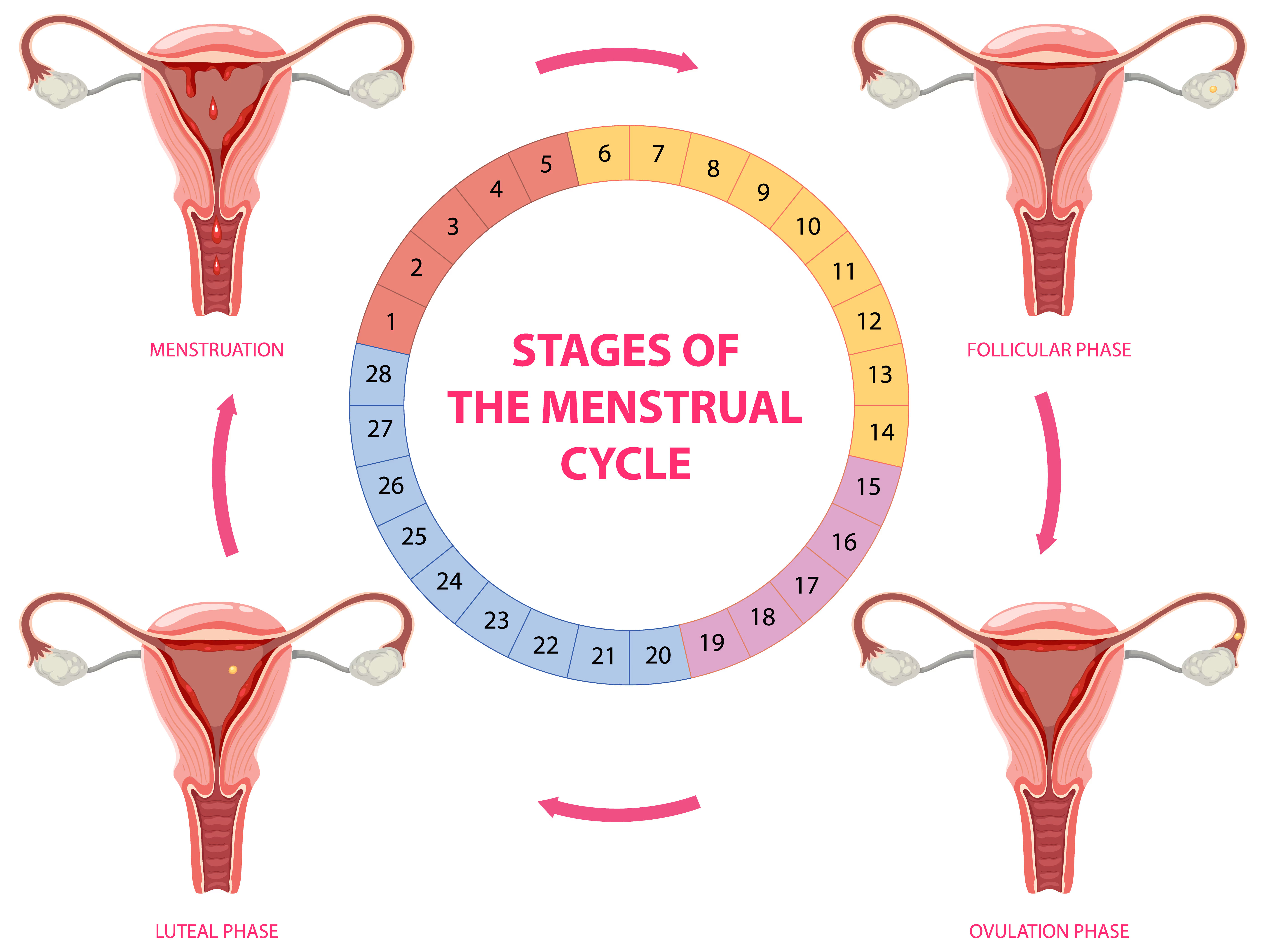
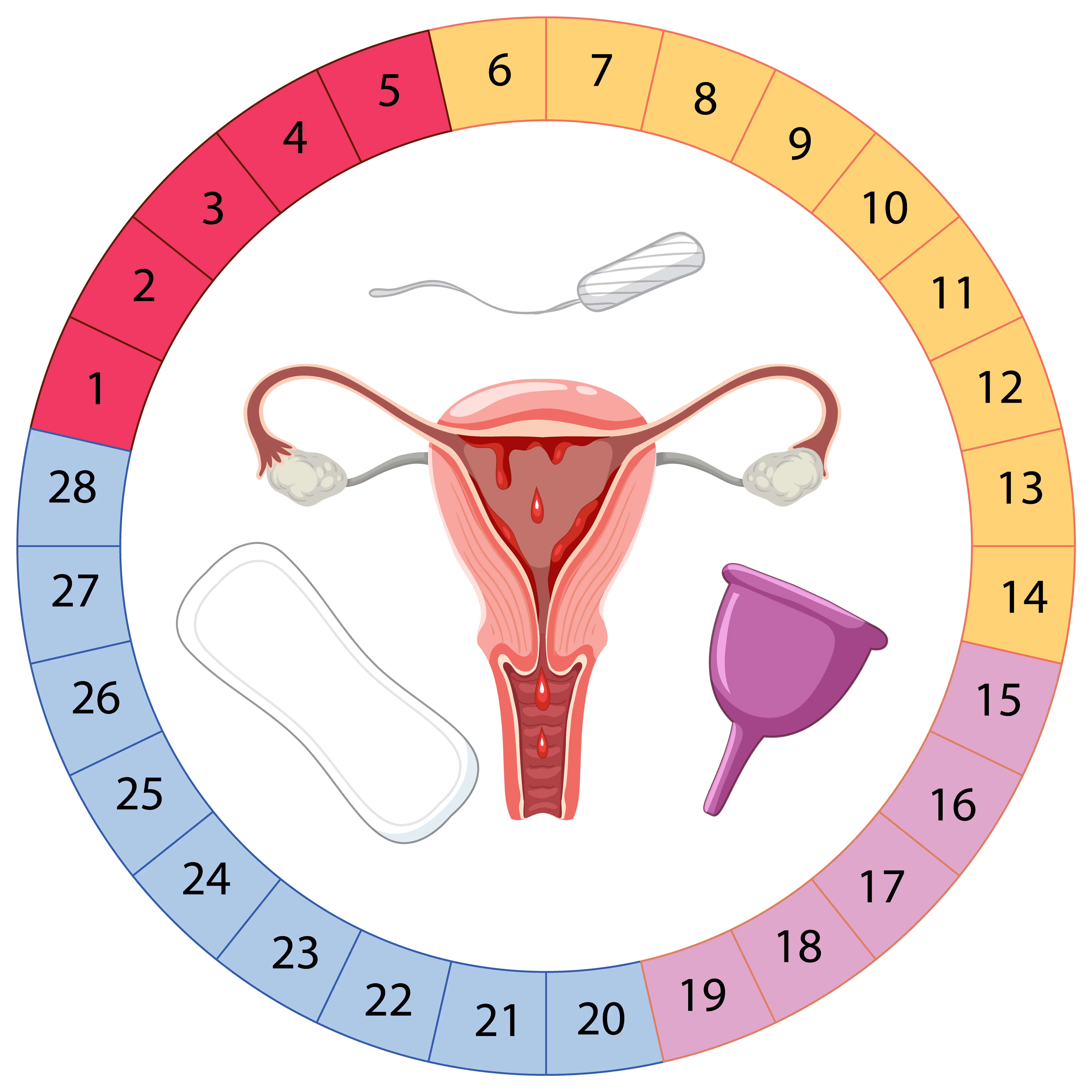
The menstrual cycle consists of three main phases: the follicular phase, ovulation, and the luteal phase. The luteal phase typically lasts between 12 and 14 days, during which progesterone levels rise to maintain a thick uterine lining (endometrium). If pregnancy does not occur, progesterone levels drop, leading to menstruation. However, in cases of LPD, this phase is often shorter than usual, and progesterone production is insufficient, preventing the endometrium from fully maturing.
There is no single cause of LPD, but several factors can contribute to this condition:
The primary cause of LPD is inadequate progesterone secretion from the corpus luteum. This deficiency prevents the endometrium from developing properly, making it less receptive to embryo implantation.
In some cases, even if progesterone levels appear normal, the uterine lining may not respond appropriately to the hormone, leading to insufficient thickening.
Disruptions in other hormone levels, such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), or estrogen, can interfere with ovulation and corpus luteum function, indirectly contributing to LPD.
Conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, and elevated prolactin levels (hyperprolactinemia) can all interfere with progesterone production and contribute to LPD.
Chronic stress can lead to elevated cortisol levels, which may suppress reproductive hormones and disrupt the menstrual cycle, leading to a shortened or dysfunctional luteal phase.
Women with very low body fat or those who engage in intense physical training may experience menstrual irregularities, including shortened luteal phases and inadequate progesterone production.
As women age, their ovarian function declines, which can lead to weaker ovulation and reduced progesterone output, contributing to LPD.
Women with LPD may experience a variety of symptoms, including:
There is no single test that definitively diagnoses LPD, but doctors may use a combination of assessments:
Keeping a record of menstrual cycle length and ovulation patterns using basal body temperature charts or ovulation predictor kits can provide insight into luteal phase duration.
Blood tests measuring mid-luteal progesterone levels can help determine whether a woman’s progesterone production is sufficient to support implantation.
A biopsy of the uterine lining can be performed to assess whether the endometrium is maturing properly during the luteal phase.
Transvaginal ultrasounds can track follicular development and endometrial thickness throughout the cycle to evaluate uterine receptivity.
Treating LPD typically involves correcting hormonal imbalances and ensuring adequate progesterone support. Treatment options include:
One of the most common treatments for LPD is progesterone supplementation, which can be administered in various forms:
For women with irregular ovulation, medications such as clomiphene citrate or letrozole can stimulate ovulation and improve luteal function.
In some cases, hCG injections may be used post-ovulation to stimulate the corpus luteum to produce more progesterone.
If LPD is linked to thyroid dysfunction, PCOS, or elevated prolactin, treating these conditions can help restore a normal luteal phase.
Improving overall health can have a positive impact on hormonal balance:
Women with LPD can still conceive and carry a pregnancy to term with proper management. However, early diagnosis and treatment are crucial, especially for those experiencing recurrent pregnancy loss or unexplained infertility. If natural conception remains challenging, assisted reproductive techniques such as intrauterine insemination (IUI) or in vitro fertilization (IVF) may be recommended.
Luteal Phase Defect is a treatable condition, but recognizing its symptoms and seeking medical evaluation is essential for women trying to conceive. Since LPD is often a sign of an underlying hormonal imbalance, addressing the root cause is key to improving reproductive health. With proper medical intervention and lifestyle modifications, many women with LPD can successfully achieve and maintain a healthy pregnancy.